Not 9, But 99
Helen Haddick, Homeland Hospice Nurse, has a gift of expression. We are grateful to her for allowing us to share the following article from her blog “From Saving to Sending, Hospice Isn’t Just About Dying.” Prior to becoming a Hospice Nurse, Helen’s journey included ten years of being a Med Surg, ICU, and Perianesthesia Nurse.
>>>
 She was the type of old lady I want to be. She was sassy and opinionated. Mostly confused but, had moments of crystal lucidity. Her eyes were set on a fellow resident and no amount of reasoning could dissuade her that this was going to be her boyfriend. She loved Diet Coke, but, fountain only please… Her accomplishments were many in life during a time when such feats were limited to those with an Adam’s apple.
She was the type of old lady I want to be. She was sassy and opinionated. Mostly confused but, had moments of crystal lucidity. Her eyes were set on a fellow resident and no amount of reasoning could dissuade her that this was going to be her boyfriend. She loved Diet Coke, but, fountain only please… Her accomplishments were many in life during a time when such feats were limited to those with an Adam’s apple.
Gold hoops were always glimmering from her ears. A former hairdresser, the hairdo was never in question. Sometimes she loved me and other days she would look at me, questioning loudly “What in the hell are you doing here?”
We shared chocolate bars and man stories. She always told me that while other parts might not work, her eyes never stopped. As her mind allowed, we talked about trash reality tv. She was my patient for a long time. Far longer than is usual for hospice. I had a nickname for her, only known to me, Kitty.
Just as Medicare requirements dictate, we had several team meetings and the talks of discharge would go round and round. But, just as the time would grow closer, something wildly unexpected would occur and discharge became a non possibility.
As rapidly as her descent was, her resurrection was equally as fast. Non responsive for days, she would just open her eyes as if she never skipped a beat. To say that this made me feel clueless would be an understatement. Just as I prepared family, boom, she was roaring right back.
I had begun to accept my lack of knowledge and power. Just as discharge talk began, the crisis began. Making sure to prepare family just in case, I found myself disbelieving they words I was uttering to them. Guiding them through the journey of end of life, I was expecting to receive calls daily that she had sat up and was demanding food.
This time was different. There was a little nagging voice urging me to keep my eyes open. There was gurgling. There was lack of waking up. My comforting and preparation of her daughter continued, even though I still felt beyond skeptical. The mottling. The fever. And yet, she had bounced back before.
Her preacher came and along with the daughter said some prayers. I had asked him to go today… nagging feeling. My phone rang as I was with another patient and noting the number, my thought was that I probably had forgotten my stethoscope there – pretty typical.
“Helen… it happened.”
“What happened?”
She
Was
Gone
With my best attempts as hiding my shock failing, I wrapped up my visit and headed over to pronounce. Even still, I half expected to walk in and a deep sleep to have been misread as an eternal sleep.
But, she was no longer.
Her face peaceful. Her life lived her way. Her journey traveled her way. Her death beyond question on her terms.
There were moments it felt she had 99 lives. That ended today.
As my heart continues to swell with gratitude which express as tears from my eyes, I cannot believe my good luck.
Her 99 lives have given such profound meaning to my one.
Homeland Hospice is a hospice program that serves 14 communities throughout Central Pennsylvania by providing end-of-life care either in a person’s home or wherever they reside, including nursing facilities. Homeland Hospice also provides bereavement support to families for a full 13 months following the death of their loved one. This service is available to anyone in the community who is experiencing grief.
To learn more, please contact Homeland Hospice at (717) 221-7890.


 About 6 years ago, I was fortunate to be able to retire from a long career as a health care lawyer. After I retired I had to figure out what I wanted to do when I “grew up.” I decided I wanted to work directly with patients instead of working at a desk. While it was definitely not easy to find such a job without any experience and with my “maturity” eventually I was hired as a nurse’s aide in the Neurology Unit at Harrisburg Hospital. This was great because they provided the training I needed for the job. Being a nurse’s aide was about as different from a legal desk job as any job could be! It was fast paced, hands on, and never a dull moment! It provided me the opportunity to meet all types of people, from all walks of life and many cultures, to provide hands-on care and comfort, and to be a part of the patients’ and their families’ lives for a short period of time. Often, patients were so grateful for my small service that it was overwhelming to me. I learned so much about people and the world in general. It was one of the most meaningful experiences of my life.
About 6 years ago, I was fortunate to be able to retire from a long career as a health care lawyer. After I retired I had to figure out what I wanted to do when I “grew up.” I decided I wanted to work directly with patients instead of working at a desk. While it was definitely not easy to find such a job without any experience and with my “maturity” eventually I was hired as a nurse’s aide in the Neurology Unit at Harrisburg Hospital. This was great because they provided the training I needed for the job. Being a nurse’s aide was about as different from a legal desk job as any job could be! It was fast paced, hands on, and never a dull moment! It provided me the opportunity to meet all types of people, from all walks of life and many cultures, to provide hands-on care and comfort, and to be a part of the patients’ and their families’ lives for a short period of time. Often, patients were so grateful for my small service that it was overwhelming to me. I learned so much about people and the world in general. It was one of the most meaningful experiences of my life. Having grown up in the dry climate of Mexico, Reynaldo (Rey) Villarreal, chaplain for Homeland Hospice, reveres the rolling hills and green trees of Central Pennsylvania. For Rey, life with Homeland Hospice is another chapter in his story of serving others in their time of need. Homeland Hospice is a hospice program that serves communities throughout Central Pennsylvania.
Having grown up in the dry climate of Mexico, Reynaldo (Rey) Villarreal, chaplain for Homeland Hospice, reveres the rolling hills and green trees of Central Pennsylvania. For Rey, life with Homeland Hospice is another chapter in his story of serving others in their time of need. Homeland Hospice is a hospice program that serves communities throughout Central Pennsylvania. We may not have control over the normal aging process or our genetic make-up, but we do have control over our lifestyles and the environment in which we choose to live. The following four lifestyle choices can greatly increase our chance of a healthy strong body as well as decrease our risk for disease and dementia:
We may not have control over the normal aging process or our genetic make-up, but we do have control over our lifestyles and the environment in which we choose to live. The following four lifestyle choices can greatly increase our chance of a healthy strong body as well as decrease our risk for disease and dementia: After a temporary pause due to the COVID-19 pandemic, Homeland Hospice is excited to announce its “Guitars … with Gratitude … 2020 Tour” is back on the road. Guitars are currently on display at Café 1500 in Harrisburg and Desperate Times Brewery in Carlisle.
After a temporary pause due to the COVID-19 pandemic, Homeland Hospice is excited to announce its “Guitars … with Gratitude … 2020 Tour” is back on the road. Guitars are currently on display at Café 1500 in Harrisburg and Desperate Times Brewery in Carlisle. Patrons visiting Desperate Times Brewery can admire Judy Dooley’s butterfly-themed guitar created in honor of her mother Rose, who died more than two years ago. In her end of life journey, Rose received in-home care support including massage and music therapy, and spiritual counseling from Homeland Hospice. The Homeland team also helped Judy as a caregiver and grieving daughter.
Patrons visiting Desperate Times Brewery can admire Judy Dooley’s butterfly-themed guitar created in honor of her mother Rose, who died more than two years ago. In her end of life journey, Rose received in-home care support including massage and music therapy, and spiritual counseling from Homeland Hospice. The Homeland team also helped Judy as a caregiver and grieving daughter. “I knew the designs would be good,” says Ed Savage, Assistant Director of Development for Homeland Center. ”But I was blown away by the creativity. The guitars are outstanding.”
“I knew the designs would be good,” says Ed Savage, Assistant Director of Development for Homeland Center. ”But I was blown away by the creativity. The guitars are outstanding.”
 The Memory Walk was the brainchild of Brian Medkeff-Rose, Homeland Hospice Bereavement Counselor, to focus on “remembrance” and to use the herb rosemary as the thread. Rosemary is symbolic for remembrance. It comes from Latin meaning “dew of the sea,” because it grows along the rocky coast of the Mediterranean. William Shakespeare references rosemary in several of his plays including Hamlet. Hamlet’s love interest, Ophelia says, “There’s rosemary, that’s for remembrance, pray for love, remember.”
The Memory Walk was the brainchild of Brian Medkeff-Rose, Homeland Hospice Bereavement Counselor, to focus on “remembrance” and to use the herb rosemary as the thread. Rosemary is symbolic for remembrance. It comes from Latin meaning “dew of the sea,” because it grows along the rocky coast of the Mediterranean. William Shakespeare references rosemary in several of his plays including Hamlet. Hamlet’s love interest, Ophelia says, “There’s rosemary, that’s for remembrance, pray for love, remember.” What made this event meaningful?
What made this event meaningful? Loneliness affects more than 42 million older Americans according to the American Psychological Association. While living alone does not inevitably lead to loneliness, it can be a contributing factor. Social contact typically decreases with age due to retirement, spouse and friends dying or moving away, lack of mobility and physical limitations. When an entire peer group is experiencing these naturally occurring changes it is easy to see why there is a decline in the number and quality of relationships as we age.
Loneliness affects more than 42 million older Americans according to the American Psychological Association. While living alone does not inevitably lead to loneliness, it can be a contributing factor. Social contact typically decreases with age due to retirement, spouse and friends dying or moving away, lack of mobility and physical limitations. When an entire peer group is experiencing these naturally occurring changes it is easy to see why there is a decline in the number and quality of relationships as we age. My father-in-law died three years ago in June. The final weeks leading up to his passing were particularly challenging in terms of providing for his needs. Thankfully, my wife and I were able to find and engage the services of an area hospice. I came away with a deep appreciation of the passion and commitment that it takes to work for a hospice – not only as a paid caregiver, i.e., nurse, social worker, but also as a volunteer. It was through that experience that I was lead to become a hospice volunteer.
My father-in-law died three years ago in June. The final weeks leading up to his passing were particularly challenging in terms of providing for his needs. Thankfully, my wife and I were able to find and engage the services of an area hospice. I came away with a deep appreciation of the passion and commitment that it takes to work for a hospice – not only as a paid caregiver, i.e., nurse, social worker, but also as a volunteer. It was through that experience that I was lead to become a hospice volunteer.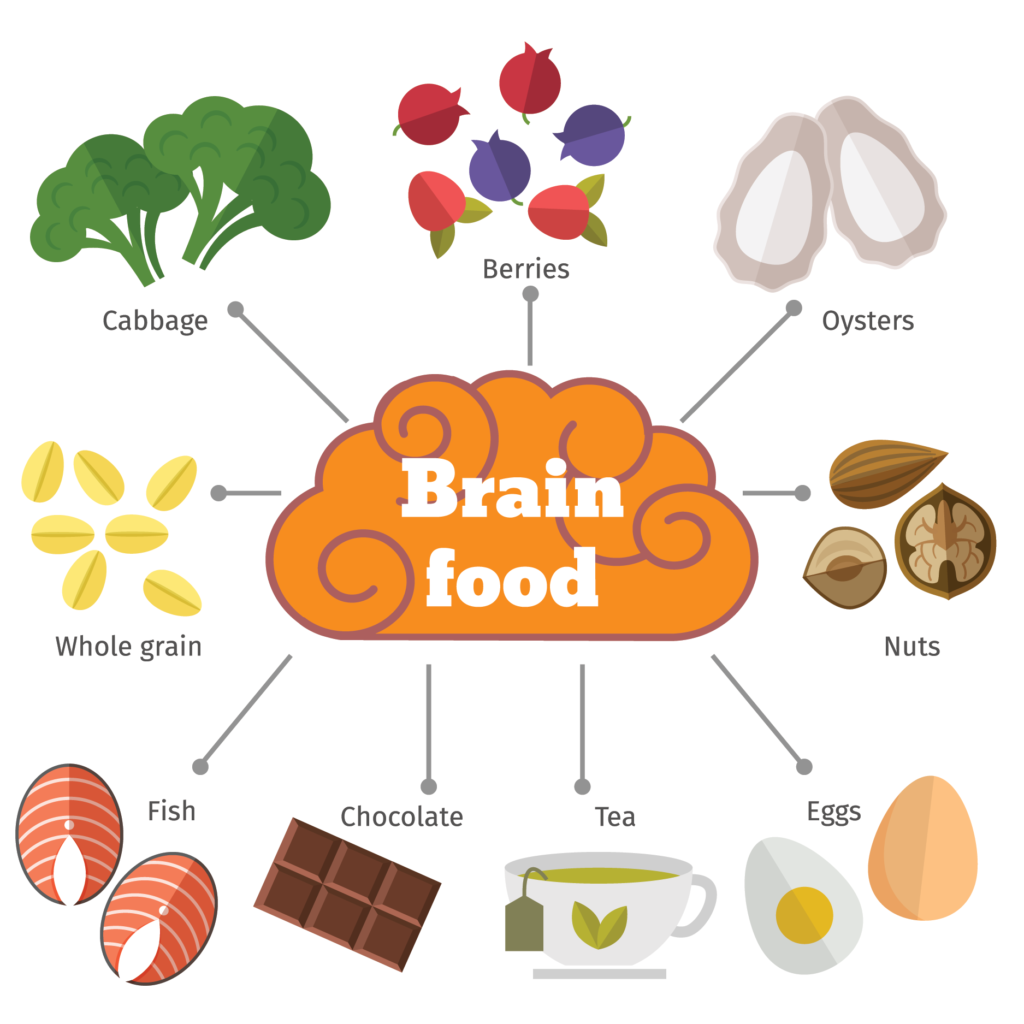

 “There are good things happening in this world,” Laurie says. “Sending cards to patients is a great way to lift their spirits while also enabling people to take part in a positive activity during a difficult time.”
“There are good things happening in this world,” Laurie says. “Sending cards to patients is a great way to lift their spirits while also enabling people to take part in a positive activity during a difficult time.”
